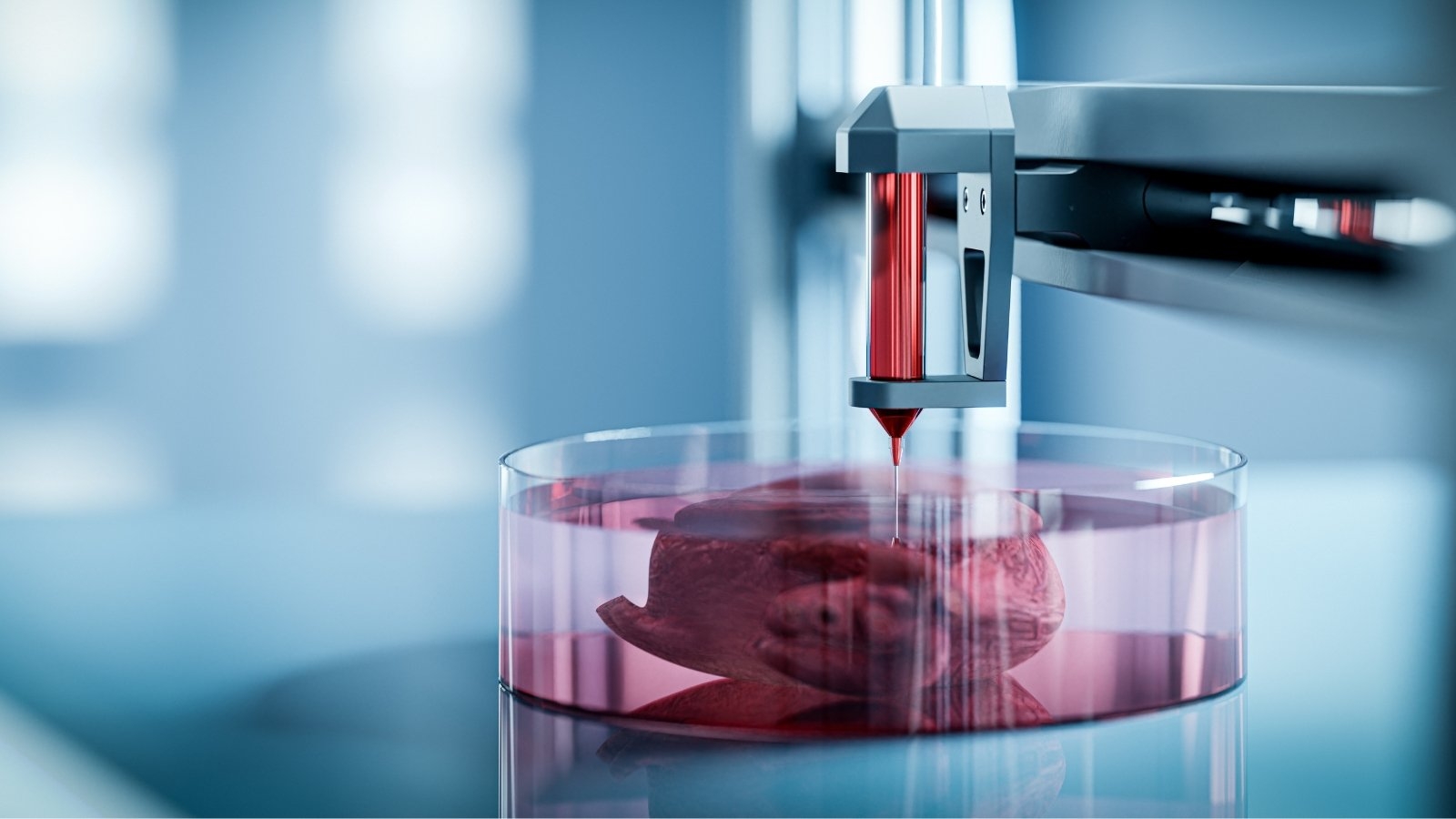
The medical community is paying more and more attention to 3D printing, a technology that was once hailed for its ability to facilitate production and prototyping, as it relates to the replacement of organs. By using additive manufacturing techniques to create viable biological tissues, the notion of 3D-printed organs has the potential to revolutionize transplantation medicine and provide patients who are suffering from organ failure fresh hope.
Fundamentally, 3D-printed organs use a technique called bioprinting. This cutting-edge method creates three-dimensional tissue constructs by using bio-inks, which are specialized materials made of live cells, growth hormones, and other biomolecules. Scientists may create complex tissues and perhaps complete organs that closely resemble the anatomical and functional properties of actual human organs by stacking these bio-inks in exact patterns.
The possibility of using 3D-printed organs to alleviate the organ scarcity is one of their biggest benefits. Thousands of people wait patiently for transplants each year, frequently with little guarantee of a transplant’s success. This issue could be resolved by 3D printing, which offers an almost infinite supply of organs that are customized to meet the demands of specific patients. Because 3D printing allows for customisation, these organs may be made to precisely match the patient’s anatomical structure, which may increase transplant success rates and lower the chance of organ rejection.
Furthermore, the development of 3D-printed organs might advance drug testing and medical research. In a safe, highly relevant environment, researchers may build patient-specific models to examine the course of a disease and evaluate the effectiveness of novel therapies. This individualized approach can help us better understand complicated diseases and expedite the discovery of novel medicines.
Still, there are a number of obstacles in the way of the field of 3D-printed organs, despite its promise. The difficulty of simulating the complex architecture and functioning of natural organs is a significant obstacle. Even while scientists have made progress printing more basic tissues like skin and cartilage, it is still very difficult to print completely functioning organs with intricate circulatory networks and cell kinds. The key to an organ’s effective integration and functioning in the human body is the capacity to print it with the cellular architecture and functions that it needs.
The ethical and regulatory environment surrounding 3D-printed organs presents another difficulty. Thorough testing and validation are necessary to guarantee the safety and effectiveness of these new constructions. In addition, rigorous evaluation of ethical problems pertaining to the use of stem cells and the modification of biological tissues is necessary to guarantee the responsible development and use of these technologies.
To sum up, 3D-printed organs are a revolutionary development in medical science that might improve research, change organ transplantation, and give patients individualized care. But realizing these advantages will come with a lot of technological, legal, and moral obstacles to overcome. The idea of 3D-printed organs being a common practice in medicine is getting closer to reality as research and technology develop, which might mean a better future for patients in need of life-saving transplants.